How a Back Injury Affects Your Life I Best Physiotherapy
According to the European Guidelines for the prevention of low back pain, it is defined as “pain and discomfort, localized below the costal margin and above the inferior gluteal folds, with or without leg pain.” Similarly, S. Kinkade describes low back pain as “pain that occurs posteriorly in the region between the lower rib margin and the proximal thighs.” Low back pain (LBP) is the fifth most common reason for physician visits, affecting nearly 60-80% of people at some point in their lives. Studies indicate that up to 23% of adults worldwide suffer from chronic low back pain, with a one-year recurrence rate ranging from 24% to 80% in this population. Physiotherapy is widely recognized as one of the most effective non-surgical treatments for managing low back pain, particularly chronic low back pain. Hence, you must reach the best physiotherapy nearby to get management for your back injury.
Types of low back pain
1.Specific low back pain
Specific low back pain refers to pain that can be attributed to a specific cause or condition affecting the structures in the lower back region.
2. Herniated Disc
A herniated disc occurs when the soft inner core of a disc in the spine leaks out through the outer portion, irritating nearby nerves and causing pain, numbness, or weakness.
3. Spinal Stenosis
Spinal stenosis is a narrowing of the spaces within the spine, which can put pressure on the spinal cord and nerves, leading to pain, numbness, or weakness.
4. Spondylolisthesis
This condition occurs when one vertebra slips forward over the one below it, which can compress the nerves and cause low back pain and possibly leg pain.
5. Degenerative Disc Disease
This is a condition where the discs in the spine break down due to age or injury, causing pain due to irritation of the nerves.
6. Compression Fractures
Fractures in the vertebrae due to osteoporosis or trauma can cause sudden onset of severe pain.
7. Ankylosing Spondylitis
This is a type of arthritis that primarily affects the spine, causing inflammation and pain.
8. Infections or Tumors
Infections of the spine (e.g., osteomyelitis) or tumors in the spine can cause localized pain in the lower back.
9. Muscle or Ligament Strain
While this is more common in non-specific low back pain, specific causes like traumatic injury or overuse can lead to strains or sprains that cause pain.
10. Sacralization or Lumbarization
These are congenital abnormalities where there is an abnormal number of vertebrae or abnormal fusion of vertebrae, which can lead to pain and dysfunction.
11. Non-specific low back pain
Non-specific low back pain is defined as pain in the lower back that is not attributed to any recognizable or known specific pathology. It is the most common type of low back pain and is typically diagnosed after specific causes, such as herniated discs, fractures, or infections, have been ruled out through diagnostic testing. It is further classified based on duration. Low back pain is categorized into three subtypes based on duration: acute, sub-acute, and chronic. Acute low back pain lasts less than 6 weeks, sub-acute lasts between 6 and 12 weeks, and chronic persistence lasts for 12 weeks or more. Low back pain that lasts longer than three months is considered chronic.
Non-specific low back pain accounts for over 90% of patients presenting to primary care and represents the majority of individuals seeking physiotherapy for low back pain. Physiotherapy assessment aims to identify impairments that may have contributed to the onset of pain or increased the likelihood of developing persistent pain. These impairments include biological factors (e.g., weakness, stiffness), psychological factors (e.g., depression, fear of movement, catastrophization), and social factors (e.g., work environment) [20]. The assessment does not focus on identifying anatomical structures (e.g., the intervertebral disc) as the source of pain.
How a back injury affects your life
Depression and Mood Swing
Chronic back pain can have a significant emotional impact over time. The ongoing struggle with pain and uncertainty about improvement can lead to serious emotional issues such as depression, anger, anxiety, and mood swings. While occasional emotional distress is normal, persistent issues need to be addressed. Engaging in activities you enjoy, as long as they don’t cause pain, can help distract from the discomfort. Exploring stress-relief activities can also be beneficial. If pain continues, consider joining a support group to find relief through sharing experiences with others who understand.
Low Self-Esteem
Chronic back pain can disrupt daily life and hinder activities you enjoy, leading to lowered self-esteem. It’s crucial to change this mindset as soon as possible. Although it may seem challenging, recognizing your inherent worth is essential. Chronic back pain does not define your identity. If low self-esteem remains a problem, seeking therapy and joining support groups can be very helpful.
Relationships
Chronic pain can significantly impact relationships. The physical pain and its emotional effects often cause sufferers to withdraw from social interactions. Friends might not fully grasp the extent of the struggle, leading to feelings of isolation. Family dynamics can also shift. If chronic back pain is affecting your relationships, it’s important to consult a professional about pain-management strategies or surgical options.
Signs and symptoms
- Pain in the lower back area, which may radiate into the lower extremities.
- Movement and coordination impairments.
- Difficulty maintaining a neutral position and/or difficulty maintaining standing, sitting, or lying positions, especially when pain radiates to the lower extremities.
- Carrying objects in the arms or bending can also provoke complaints.
- Daily activities such as household tasks, sports, and recreational activities can be challenging.
- When pain is widespread, the sensory experiences of the patient can also become altered.
Prevention
Primary prevention: Practices aimed at preventing low back pain before it occurs. This includes promoting regular exercise to strengthen back muscles, educating people about proper lifting techniques, and ensuring ergonomic workplace setups to reduce the risk of injury.
Secondary prevention: Actions taken to prevent recurrent episodes or worsening of low back pain after it has occurred. This includes early intervention with physiotherapy and exercise to prevent chronicity, as well as patient education on pain management techniques and strategies to avoid aggravating activities.
Tertiary prevention: Measures to improve quality of life and reduce symptoms for people with chronic low back pain. This includes providing access to pain management programs, rehabilitation services, and support groups, as well as promoting return-to-work programs and ergonomic adjustments in the workplace to facilitate functioning despite ongoing symptoms.
Physiotherapy Treatments
1. Education and Advice
- Providing information about the nature of low back pain, reassurance about the prognosis, and advice on self-management strategies.
2. Exercise Therapy
- Core Strengthening: Exercises to strengthen the abdominal and back muscles, which provide support to the spine (e.g., plank variations, bridges).
- Flexibility and Range of Motion: Stretching exercises to improve flexibility and maintain or restore normal range of motion in the spine and surrounding muscles (e.g., hamstring stretches, cat-cow stretch).
- Aerobic Conditioning: Low-impact exercises such as walking, swimming, or cycling to improve cardiovascular fitness and reduce stiffness.
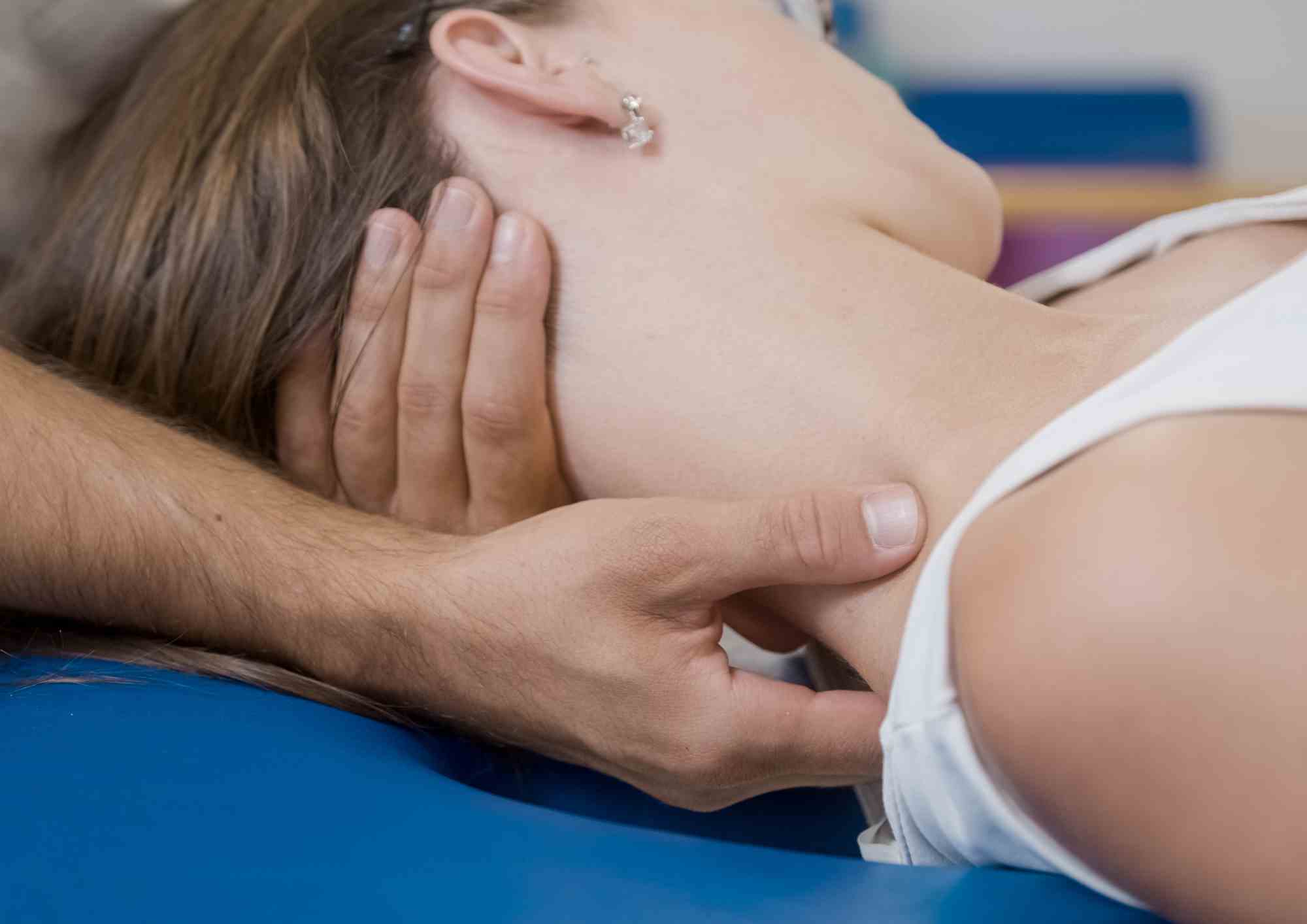
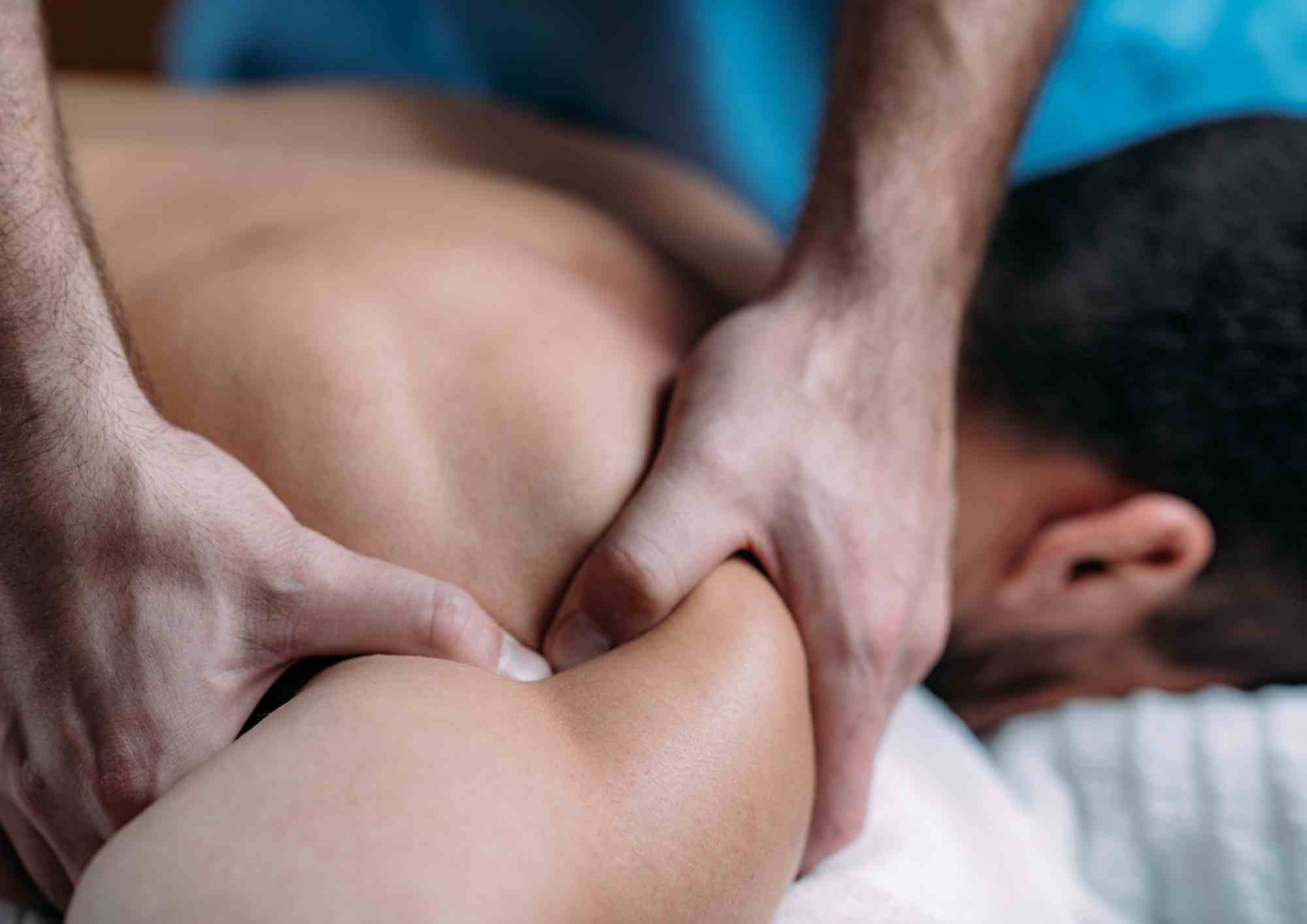
3. Manual Therapy
- Spinal Mobilization: Passive movement of spinal joints to reduce pain and improve mobility.
- Spinal Manipulation: High-velocity, low-amplitude thrusts to joints to alleviate pain and restore function (often used cautiously and selectively).
- Soft Tissue Mobilization: Massage and other hands-on techniques to relax tense muscles and improve circulation.
4. Modalities
- Heat Therapy: Applying heat packs or warm towels to the affected area to relax muscles and improve blood flow.
- Cold Therapy: Using ice packs or cold packs to reduce inflammation and numb the area, particularly in acute stages.
- Electrotherapy: Techniques such as TENS (transcutaneous electrical nerve stimulation) or ultrasound to provide pain relief and promote healing.
5. Psychological Support:
- Addressing psychological factors such as anxiety, depression, or fear of movement through cognitive-behavioral techniques and counseling.
- Encouraging relaxation techniques and stress management strategies.
6. Posture and Movement Re-Education:
- Teaching proper posture and body mechanics during daily activities, including lifting, sitting, and standing.
- Advising on ergonomic modifications at home and work to reduce strain on the spine.
7. Functional Rehabilitation
- Specific exercises and activities aimed at improving the ability to perform daily tasks and activities without pain.
- Gradual return to work or sports activities through structured rehabilitation programs.
Frequently Asked Questions (FAQs)
Preventing low back pain involves regular exercise to strengthen core muscles, maintaining proper posture, using ergonomic furniture, and practicing safe lifting techniques. Engaging in activities that promote flexibility and staying active also helps.
Physiotherapy offers a diverse array of techniques aimed at reducing pain, enhancing mobility, and strengthening the muscles supporting the spine. These techniques include electrotherapy, hot and cold packs, ultrasound therapy, manual therapy, nerve mobilization, exercise therapy, and education on proper body mechanics and posture correction. By addressing the root causes of pain and promoting healing, physiotherapy can effectively manage and treat low back pain.
You should see a physiotherapist if your back pain persists for more than a few weeks, is severe, or is affecting your daily activities. Early intervention can prevent the condition from worsening and promote faster recovery.
During a physiotherapy session, you can expect an assessment of your condition, personalized exercise plans, manual therapy, and education on posture and movement techniques. The therapist may also use modalities like heat, cold, or electrotherapy for pain relief.
Yes, physiotherapy can be effective for various types of back pain, including specific conditions like herniated discs, spinal stenosis, and non-specific low back pain. A tailored treatment plan can address the underlying causes and improve overall function.
Conclusion
In summary, physiotherapy for low back pain is typically individualized based on the specific needs and circumstances of each patient. The goal is to reduce pain, improve function, and enhance quality of life through a combination of these evidence-based treatments. Synapse Physiotherapy specializes in treating low back pain and is dedicated to helping individuals regain their mobility and quality of life. Addressing back pain early with professional rehabilitation can prevent it from affecting daily activities. If you have any questions or need assistance, feel free to reach out to Synapse Physiotherapy for expert care and support.
Produced by MYSense
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.