How Many Times Per Week Should You Have Physiotherapy?
If you’ve experienced an illness or injury affecting your movement or ability to perform daily activities, your doctor might have recommended seeing a physiotherapist. Physiotherapists, also known as physical therapists, specialize in helping patients improve pain management, balance, mobility, and motor function. If you’re facing such challenges, you can look up local services, such as searching for “physiotherapy Petaling Jaya,” to find treatment near you.
Have you ever wondered how often you should attend physiotherapy Petaling Jaya sessions? The ideal frequency depends on various factors, including your specific condition, the severity of the issue, and the treatment plan designed by your physiotherapist. Since physiotherapy is personalized, there’s no universal answer.
Factors That Affect the Frequency of Physiotherapy Sessions
Nature and Severity of the Condition
The type and seriousness of your condition significantly influence how often you need physiotherapy Petaling Jaya. Acute injuries or post-surgical rehabilitation often require more frequent sessions, typically two to three times a week, to address immediate concerns, manage pain, and monitor progress. Chronic conditions or long-term issues may start with a similar frequency but gradually reduce as the patient gains independence through a home exercise program or other self-management strategies.
Phase of Rehabilitation
The rehabilitation process can be divided into different phases, each requiring varying levels of physiotherapy involvement. In the initial phase, frequent sessions (e.g., twice a week) are needed to focus on pain management and early recovery. During the intermediate phase, sessions may reduce to once a week or fortnightly as the emphasis shifts to strengthening and improving mobility. In the maintenance phase, occasional sessions may be sufficient for monitoring progress and preventing relapses.
Response to Treatment
Your progress and how you respond to physiotherapy will also dictate the frequency of sessions. If you are recovering well and achieving milestones, your physiotherapist may reduce the number of visits. Conversely, if symptoms persist or worsen, more frequent sessions may be required to reassess and adjust the treatment plan.
Adherence to Home Exercise Program
Following a prescribed physiotherapy Petaling Jaya home exercise program can greatly influence the need for in-person sessions. Patients who diligently perform their exercises often require fewer sessions as they gain the tools to manage their rehabilitation independently. However, those who struggle with consistency might need more regular visits for guidance and motivation.
Pain Levels and Symptom Management
Severe or persistent pain may necessitate more frequent physiotherapy sessions to provide immediate relief and address underlying issues. As symptoms improve, the frequency of visits typically decreases.
Functional Goals and Lifestyle Demands
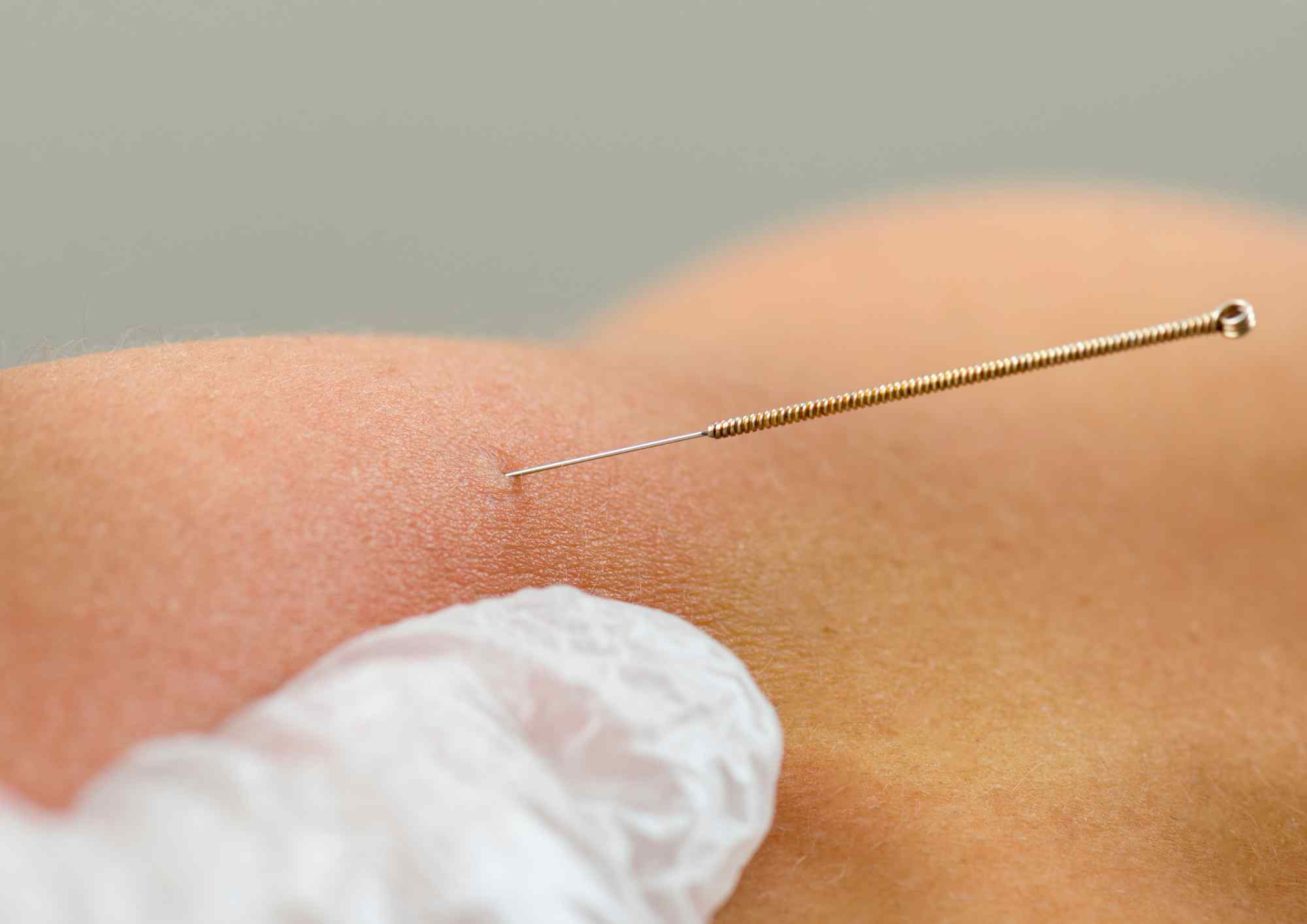
Your goals and lifestyle play an essential role in determining how often you see a physiotherapist. For instance, if you aim to return to sports or physically demanding activities, you may require more frequent sessions tailored to these objectives. Athletes preparing for competitions or events may benefit from weekly treatments, such as massage or dry needling, to optimize muscle function.
Practical Considerations
Practical factors, such as your schedule, availability, and financial resources, can influence session frequency. Physiotherapists at physiotherapy Petaling Jaya will consider these constraints and work with you to develop a feasible plan while ensuring effective treatment.
Long-Term Management and Preventative Care
In cases where physiotherapy at physiotherapy Petaling Jaya is part of a long-term management or preventative strategy, session frequency tends to be lower. Periodic check-ins, such as monthly visits, are often sufficient to maintain progress and address new concerns. Preventative care helps minimize the risk of future injuries and supports overall physical well-being.
Communication with Your Physiotherapist
Effective communication with your physiotherapist at physiotherapy Petaling Jaya is crucial in determining the appropriate frequency of sessions. Sharing updates on your condition, progress, or any concerns ensures that your treatment plan remains aligned with your evolving needs and goals. Regular adjustments based on this feedback help maximize the effectiveness of physiotherapy and promote optimal recovery.
How Often Should You Do Physiotherapy Exercises at Home?
As part of your physiotherapy plan from Synapse physiotherapy Petaling Jaya, you’ll likely be assigned exercises to complete at home between sessions to support your recovery. The frequency of these exercises depends on the specific condition and treatment goals, but here are some general guidelines:
- Low-load, low-intensity exercises: These can usually be performed daily, and in some cases, even twice a day.
- High-load, high-intensity exercises: These should be done less frequently, typically 2–3 times per week. While they are crucial for recovery, performing them too often or incorrectly can hinder progress.
If you’re uncertain about the intensity or frequency of any exercise, consult your physiotherapist at Synapse physiotherapy Petaling Jaya for guidance. They can provide tailored advice to ensure you’re performing exercises safely and effectively.
What Does A Good Physiotherapy Schedule Look Like?
A balanced schedule combines physiotherapy appointments, at-home exercises, and rest days to optimize recovery. If you attend physiotherapy 2–3 times a week, plan your home exercises on non-appointment days, leaving room for at least one rest day each week.
In conclusion, the frequency of physiotherapy exercises ultimately depends on your individual needs and condition. However, it is essential to consult with your physiotherapist to create a tailored plan that aligns with your rehabilitation goals. Commitment and adherence to this plan are crucial to achieving effective results. Start your rehabilitation journey with the experienced physiotherapists at Synapse physiotherapy Petaling Jaya to ensure you’re on the right path to recovery.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.