Dry Needling Near Me: A Non-Invasive Treatment Option
Are you searching for “dry needling near me” to relieve muscle pain and tension? Dry needling is a non-invasive, highly effective treatment used by physical therapists to target trigger points and muscle knots. Whether you’re dealing with chronic pain, sports injuries, or muscle stiffness, dry needling could be the solution you need.
What is dry needling?
Dry needling, also referred to as trigger point dry needling or intramuscular stimulation (IMS), is a specialized therapeutic technique performed by healthcare professionals such as physical therapists, physicians, chiropractors, and sports medicine specialists.
While some acupuncturists claim that dry needling is derived from traditional acupuncture, others consider it a modern variation of trigger point injections—but without the use of medication. This evidence-based practice is primarily used to relieve muscle pain, tension, and dysfunction by targeting myofascial trigger points—tight, knotted bands within muscles that can cause pain and restricted movement.
Benefits of Dry Needling
- Pain Relief: By targeting trigger points, dry needling effectively reduces muscle pain and discomfort in areas such as the neck, back, shoulders, and hips. It helps deactivate pain-inducing muscle knots, leading to long-lasting relief.
- Improved Range of Motion: The release of muscle tightness allows for greater flexibility and improved movement, making it ideal for athletes, individuals recovering from injuries, and those with mobility issues.
- Enhanced Blood Flow: The insertion of needles stimulates increased circulation to the affected muscles, promoting faster healing, reducing inflammation, and improving overall tissue repair.
- Muscle Relaxation: Dry needling directly decreases muscle tension and stiffness, helping to prevent spasms and providing a deep sense of relaxation and relief.
- Faster Recovery: By addressing the root cause of muscle pain, dry needling accelerates recovery from injuries, overuse conditions, and post-exercise fatigue, allowing individuals to return to daily activities sooner.
- Nerve Function Improvement: Research suggests that dry needling can enhance nerve communication, improving muscle control, reducing nerve-related pain, and supporting overall neuromuscular function.
What to Expect During and After a Dry Needling Session
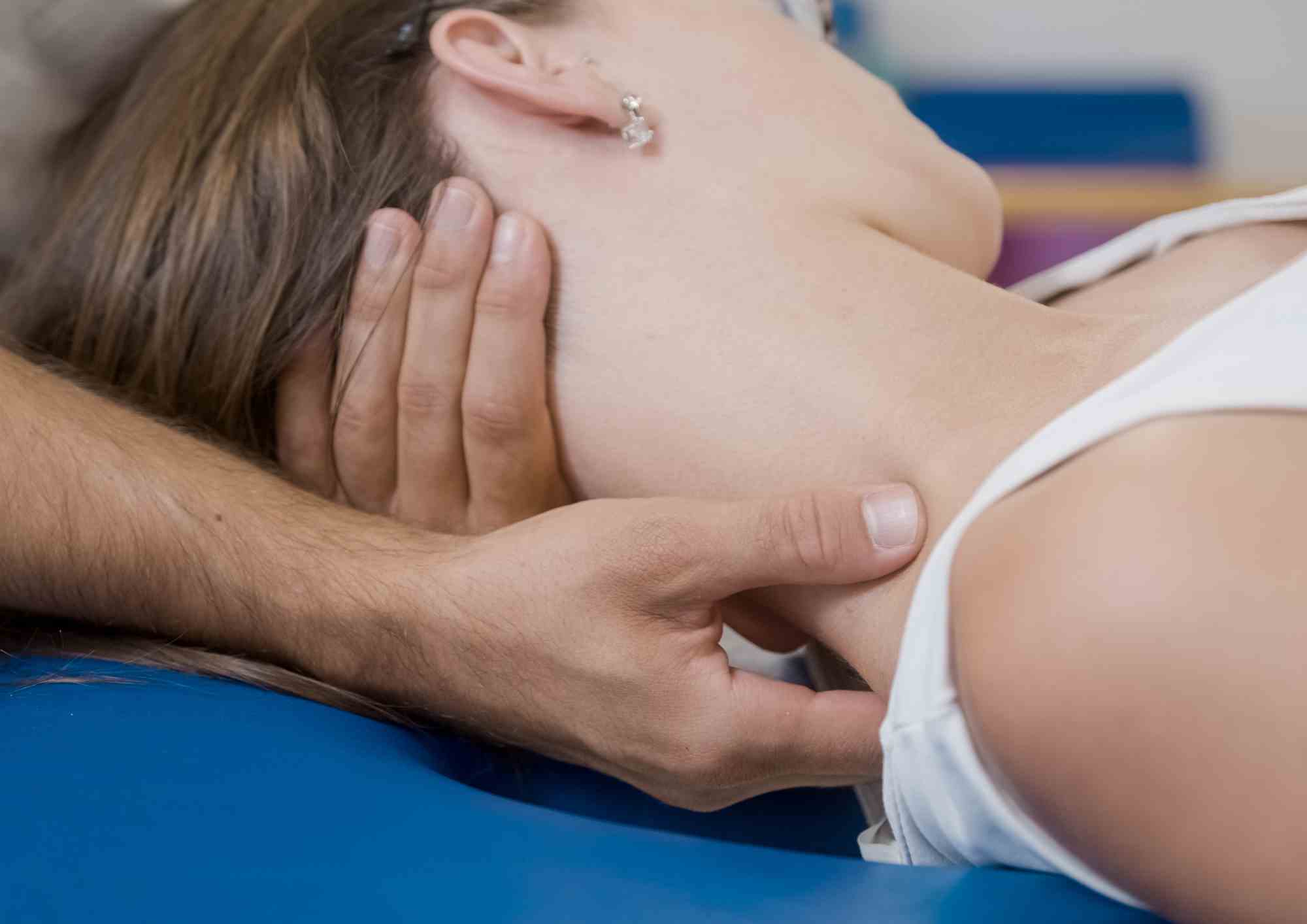
During the Dry Needling Session
A trained practitioner will carefully insert thin, sterile needles into specific muscle trigger points to release tension and alleviate pain. You may feel a slight prick or mild discomfort upon insertion, followed by a localized muscle twitch response—a quick, involuntary contraction of the muscle. This twitch is a positive sign, indicating that the trigger point has been successfully stimulated.
Once the needles are in place, they remain for a short period, typically ranging from a few seconds to several minutes, depending on the treatment plan. The practitioner may gently manipulate the needles to enhance muscle relaxation and optimize pain relief. While some temporary soreness or tingling may occur, the overall procedure is well-tolerated and does not cause significant pain.
What to Expect After a Dry Needling Session
- Mild Muscle Soreness: It is common to experience slight tenderness or soreness in the treated area, similar to delayed onset muscle soreness (DOMS) that occurs after exercise. This discomfort usually subsides within 24 to 48 hours. Applying heat, gentle stretching, and staying hydrated can help alleviate post-treatment soreness.
- Improved Flexibility & Range of Motion: Many patients notice an immediate improvement in mobility and flexibility, as dry needling releases tight muscles and reduces restrictions in movement. This makes it particularly beneficial for athletes, active individuals, and those recovering from injuries.
- Pain Reduction & Muscle Relaxation: One of the primary benefits of dry needling is its ability to relieve muscle pain and tension. While some people experience instant relief, others may feel gradual improvement over the next 24 to 72 hours as their muscles continue to relax and heal.
Dry Needling vs. Acupuncture: Understanding the Key Differences
Although dry needling and acupuncture both involve the insertion of thin needles into the body, they are fundamentally different in purpose, philosophy, and application. Understanding these differences can help you determine which treatment best suits your needs.
1. Origin and Theoretical Basis
- Dry Needling is based on Western medicine, particularly anatomy, neurophysiology, and musculoskeletal science. It is primarily used by physical therapists, chiropractors, and sports medicine practitioners to relieve muscle pain, improve movement, and enhance muscle function. Dry needling specifically targets trigger points—tight muscle knots that cause pain and dysfunction.
- Acupuncture originates from Traditional Chinese Medicine (TCM) and is rooted in the concept of Qi (pronounced “chee”), which refers to the body’s vital energy. According to TCM, imbalances in Qi flow along meridians (energy pathways) can cause illness and pain. Acupuncture aims to restore this balance by inserting needles at specific meridian points to regulate energy flow and promote overall well-being.
2. Purpose and Treatment Goals
- Dry Needling is primarily used to:
- Relieve musculoskeletal pain (e.g., muscle tightness, spasms, and trigger points)
- Improve range of motion and flexibility
- Enhance muscle recovery and athletic performance
- Reduce inflammation and improve blood circulation
- Acupuncture is traditionally used for a broader range of conditions, including:
- Chronic pain management (e.g., migraines, arthritis, fibromyalgia)
- Stress, anxiety, and emotional balance
- Digestive disorders (e.g., irritable bowel syndrome)
- Hormonal and immune system regulation
3. Needle Placement and Technique
- Dry Needling involves inserting needles directly into myofascial trigger points, which are hyperirritable spots in muscles that cause pain and tightness. The goal is to stimulate a twitch response, which helps release muscle tension and restore normal function. The practitioner may also manipulate the needles slightly to enhance the therapeutic effect.
- Acupuncture follows a structured meridian system. Needles are inserted at specific energy points along the body’s meridians to restore energy balance. The technique is generally more superficial, and needles may be left in place for 15 to 30 minutes without manipulation.
4. Sensation and Patient Experience
- Dry Needling can cause a localized twitch response, which may feel like a quick muscle contraction. Some patients experience mild soreness afterward, similar to post-exercise soreness, but this usually resolves within 24 to 48 hours.
- Acupuncture is typically gentler and more relaxing. Many patients report a tingling, warm, or calming sensation during treatment. Unlike dry needling, acupuncture does not aim to elicit a twitch response or deep muscle stimulation.
5. Conditions Treated
- Dry Needling is most effective for treating muscle-related pain and dysfunction, including:
- Neck, back, and shoulder pain
- Sports injuries and muscle strains
- Tension headaches and migraines caused by muscle tightness
- Post-surgical rehabilitation
- Tendonitis and overuse conditions
- Acupuncture is commonly used for a wider range of internal and external conditions, such as:
- Chronic pain syndromes (e.g., arthritis, fibromyalgia, nerve pain)
- Stress, anxiety, and insomnia
- Digestive issues (e.g., bloating, IBS)
- Women’s health concerns (e.g., menstrual pain, fertility support)
6. Who Performs the Treatment?
- Dry Needling is performed by licensed physical therapists, chiropractors, and medical professionals with specialized training in musculoskeletal and neuromuscular health. It is considered a medical intervention rather than an alternative therapy.
- Acupuncture is performed by licensed acupuncturists who have extensive training in Traditional Chinese Medicine and holistic healing. In some cases, medical doctors, naturopaths, or chiropractors with additional acupuncture training may also provide treatment.
Which One Is Right for You?
- Choose Dry Needling if:
✔ You have muscle pain, stiffness, or trigger points causing discomfort.
✔ You need faster muscle recovery and improved movement.
✔ You are dealing with sports injuries, postural issues, or musculoskeletal pain. - Choose Acupuncture if:
✔ You want to address chronic pain, stress, or energy imbalances.
✔ You are looking for a holistic approach to overall well-being.
✔ You need support for internal conditions like digestion, immunity, or hormonal balance.
Is Dry Needling Safe? How to Find a Specialist Near You
Yes! When performed by a licensed and trained practitioner, dry needling is a safe, minimally invasive, and effective therapy for relieving muscle pain, improving mobility, and promoting recovery. To ensure the best results, it’s essential to find a qualified specialist in your area.
How to Find a Trusted Dry Needling Specialist Near You
If you’re searching for “dry needling near me”, consider checking the following:
- ✅ Physical therapy clinics that offer specialized dry needling treatment plans.
- ✅ Chiropractic centers with trained professionals experienced in dry needling techniques.
- ✅ Online reviews and testimonials to find top-rated providers with proven success.
Conclusion
Dry needling is a safe, effective, and minimally invasive therapy when performed by a trained and licensed professional. It offers significant benefits for relieving muscle pain, improving mobility, and enhancing recovery. If you’re looking for expert care, Synapse Physiotherapy employs highly trained and qualified physiotherapists who specialize in dry needling to provide personalized treatment tailored to your needs.
Contact us today to learn more about how dry needling can help you achieve relief and regain optimal movement. Our team is ready to assist you on your journey to better health and well-being.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.