How Physiotherapy Helps With Badminton Injuries
Introduction
Badminton is a non-contact individual sport generally regarded as very safe since it doesn’t involve direct physical interaction with other players. However, the quick direction changes, jumps, lunges at the net, and fast arm movements needed to hit the shuttlecock from various postures can raise the risk of injury. Research has shown that taking part in badminton training and tournaments increases the likelihood of injury by 15 to 39%. Interestingly, the injury rate is higher during training than in competition. In this context, physiotherapy plays a crucial role in treating such sports injuries. Sports physiotherapy, in particular, offers specialized rehabilitation programs designed for athletes recovering from injuries. These tailored treatments help athletes regain their strength and return to their sport in optimal condition.
Common badminton injuries and ways to prevent
1. Anterior cruciate ligament injury.
One of the most serious and potentially game-altering injuries is an ACL tear (anterior cruciate ligament). Similar to an ankle sprain, ACL injuries typically occur from rapid twisting movements in response to an opponent’s shot. This happens when the foot remains planted on the ground while the body twists with significant force and weight before the foot has a chance to move. In a fast-paced game like badminton, this is an easy mistake to make. While some cases may not require surgery, most do. Undoubtedly, an ACL injury is among the most severe injuries a badminton player can ever experience.
Injuries can never be completely avoided, as they are an inherent part of both sports and life. However, learning proper footwork can significantly reduce the risk of sustaining an ACL injury. Additionally, a proper warm-up is essential. Getting the blood flowing through all the muscles helps reduce stiffness and improve flexibility, lowering the likelihood of injury.
2. Achilles Tendonitis
Achilles tendonitis is an overuse injury that affects the Achilles tendon, which links the calf muscles to the heel bone. It often results from repetitive jumping and sudden directional changes. Common symptoms include pain and swelling at the back of the heel. If you suspect an Achilles rupture due to these symptoms, it is important to seek medical attention. An ultrasound or MRI can help determine the severity of the injury.
To help prevent injuries, it’s important to incorporate a proper warm-up routine, including dynamic stretches and warm-up exercises, before playing. Wearing appropriate footwear with good support and cushioning also plays a key role in injury prevention. Additionally, strengthening the calf muscles through targeted exercises can further reduce the likelihood of injury, particularly to areas like the Achilles tendon.
3. Ankle sprain
Ankle sprains are the most common injuries among badminton players, occurring when the ligaments in the ankle are overstretched or torn. This injury often happens due to the rotational movements at the ankle during quick lateral motions or after landing from strokes. Common symptoms include pain, swelling, bruising, and difficulty walking.
To prevent ankle sprains in badminton, it’s important to wear proper footwear, specifically badminton shoes that offer good ankle support and traction. Additionally, performing dynamic stretches and warm-up exercises before playing helps prepare the body for intense activity. Strengthening the muscles around the ankle is also crucial for reducing the risk of injury.
4. Rotator cuff injury (shoulder pain)
Overhead shots in badminton can lead to damage to the rotator cuff in the shoulder. Even with proper racket handling, players may still suffer from repetitive stress injuries due to overuse or repeatedly practicing the same shot. Common symptoms of rotator cuff injuries include pain, stiffness, and weakness in the shoulder.
To reduce the risk of shoulder injuries in badminton, it’s essential to strengthen the shoulder blade and rotator cuff muscles. Maintaining flexibility in the shoulder joint is also important for injury prevention. Additionally, improving spine mobility and core strength contributes to delivering precise shots. Using proper technique and form while playing helps avoid excessive strain on the shoulder.
5. Wrist pain
Wrist sprains are common in badminton because of the repetitive wrist movements required to hit the shuttlecock. Symptoms often include pain, swelling, and a limited range of motion. These sprains typically occur due to improper hand positioning or an incorrect grip. Additionally, some wrist injuries can result from sudden forces and changes in movement, leading to acute injuries.
To prevent wrist sprains in badminton, it’s crucial to use proper technique by ensuring the correct grip and form to avoid excessive strain on the wrist. While playing, maintain a loose grip; the thumb should wrap around the handle rather than lie straight along the shaft. Additionally, performing dynamic stretches and warm-up exercises before playing helps prepare the wrist for activity. Strengthening the wrist muscles through targeted exercises is also essential for injury prevention.
Physiotherapy for the injuries
Physiotherapy provides a focused approach to managing and recovering from badminton injuries:
- Individualized Assessment: A physiotherapist performs a comprehensive evaluation of your injury, movement patterns, and overall physical condition to develop a personalized treatment plan.
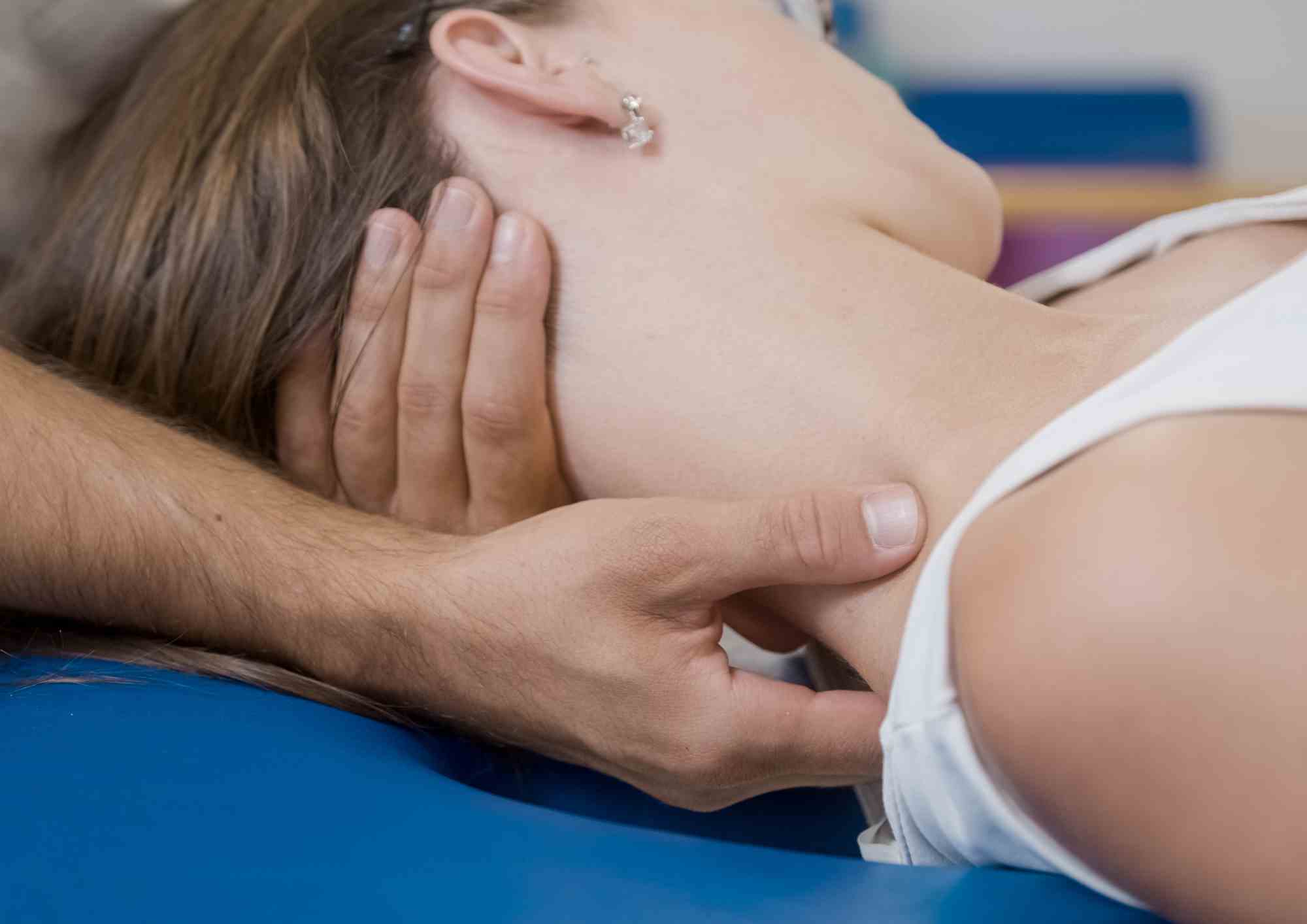
- Manual Therapy: Techniques such as joint mobilizations, massage, and trigger point release can help alleviate pain, reduce inflammation, and enhance mobility.
- Rehabilitation Exercises: A physiotherapist will create a rehabilitation program aimed at strengthening weak areas, improving flexibility, and restoring function based on your specific injury and needs.
- Education: Physiotherapists offer essential education on proper techniques, injury prevention strategies, and safe practices to help minimize the risk of future injuries.
- Recovery and Prevention Plans: Alongside treating current injuries, physiotherapists assist in creating a plan to prevent recurrence, which includes advice on warm-up routines, recovery strategies, and progressive training.
Ankle Sprains
- Acute Phase: Apply R.I.C.E (Rest, Ice, Compression, Elevation) and take anti-inflammatory medications.
- Sub-Acute Phase: Start with gentle range of motion exercises and focus on balance and proprioception training.
- Rehabilitation Phase: Include strengthening exercises for the ankle muscles along with sport-specific drills.
Knee Injuries
- Acute Phase: Use rest, ice, compression, elevation, and anti-inflammatory medications.
- Sub-Acute Phase: Begin gentle range of motion exercises and strengthen the quadriceps and hamstrings.
- Rehabilitation Phase: Emphasize functional training, proprioceptive exercises, plyometrics, and sport-specific drills.
Shoulder Injuries
- Acute Phase: Rest, apply ice, and take anti-inflammatory medications.
- Sub-Acute Phase: Perform gentle range of motion exercises and strengthen the rotator cuff and scapular stabilizers.
- Rehabilitation Phase: Focus on functional training, sport-specific drills, and progressive loading.
Wrist Injuries
- Acute Phase: Rest, ice, and use anti-inflammatory medications.
- Sub-Acute Phase: Conduct gentle range of motion exercises and strengthen the wrist flexors and extensors.
- Rehabilitation Phase: Concentrate on progressive loading, functional training, and sport-specific drills.
Achilles Tendinitis
- Acute Phase: Rest, apply ice, and take anti-inflammatory medications.
- Sub-Acute Phase: Engage in gentle calf muscle stretching and perform eccentric strengthening exercises.
- Rehabilitation Phase: Incorporate progressive loading, functional training, and sport-specific drills.
In conclusion, badminton is an enjoyable and healthy sport, but it’s essential to take measures to prevent and treat injuries. Always pay attention to your body and seek medical advice if you experience any pain or discomfort. Don’t let injuries keep you from enjoying the game. Physiotherapy plays a crucial role in accelerating recovery and preventing future injuries, helping you return to the court with greater strength, flexibility, and confidence. Consider booking an appointment with Synapse Physiotherapy for tailored support.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.