Physiotherapy For A Slipped Disc Or Disc Prolapse
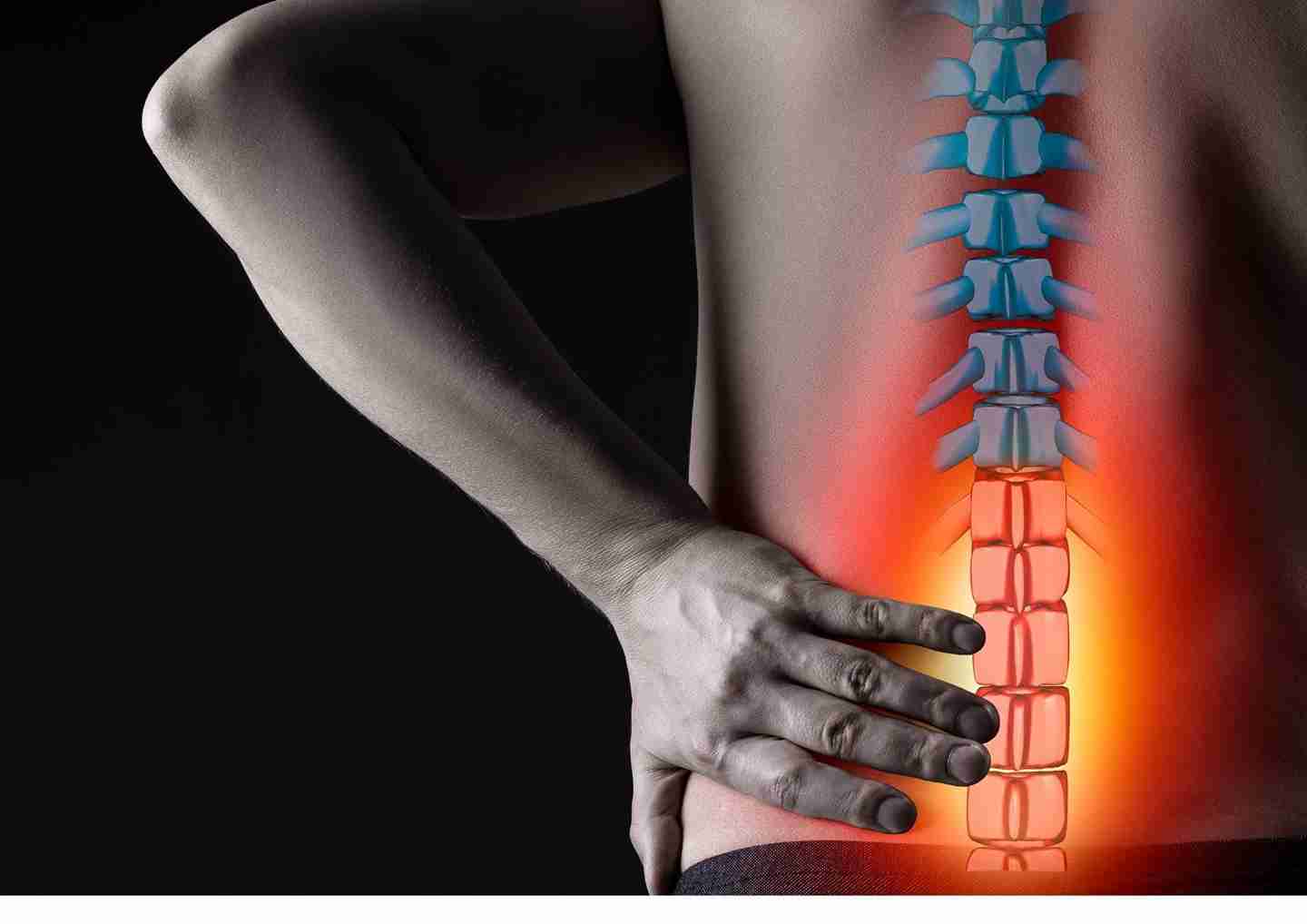
A slipped disc, often referred to as a disc prolapse or herniated disc, is a relatively common and serious spinal condition causing radicular pain (nerve-related pain) and can affect individuals of any age. Engaging in strenuous jobs, high-impact sports, or leading a sedentary lifestyle are prevalent factors that increase the likelihood of developing this disorder. Patients suffering from slipped disc issues often experience sensory and motor alterations, in conjunction with radicular pain and discomfort, leading to functional limitations.
If you are looking for physiotherapy for a slipped disc, our physiotherapist will be able to address your needs and concerns. At Synapse Physiotherapy, we offer personalized, non-invasive treatment plans to address slipped discs. Through targeted physical therapy, we aim to help our patients achieve long-term relief, improved functionality, and prevention of future injuries.
Widespread symptoms and complaints we typically target in our treatment of prolapsed spinal discs include:
a) Radicular Pain (Nerve Pain)
Depending on the degree of herniation and the location of the disc, patients often report sharp or shooting pain radiating from the lower back down to the legs (sciatica) or from the neck to the arms.
b) Numbness / Tingling
Due to nerve root compression from the herniated disc, patients may experience sensations of numbness accompanied by tingling or a prickling sensation in the arms or legs. These symptoms may be alleviated through interventions such as postural correction, spinal decompression exercises, or nerve mobilization techniques.
c) Muscle Weakness
Nerve root compression may lead to weakness in specific muscle groups. Additionally, the lack of use of these muscles contributes to further weakening. Consequently, activities such as walking, lifting, or performing daily tasks can become difficult. Customized strengthening exercises provided by our team not only helps to regain strength but also enhance neuromuscular control, promoting better communication between the nerves and muscles. This encourages recovery of muscle function, even in areas weakened by nerve compression.
d) Back/Neck Stiffness and Reduced Mobility
Due to pain and/or muscle guarding from a slipped disc, many patients experience limited mobility and stiffness in the back or neck.
e) Pain Aggravated by Movement
Increased discomfort occurs when performing spinal movements such as bending or lifting. Sitting for long periods may also lead to unpleasant pain.
f) Fatigue or Restlessness
Chronic pain and discomfort may lead to overall fatigue or restlessness, as individuals struggle to find comfortable positions or manage prolonged pain.
Synapse Physiotherapy provides customized, evidence-based treatment plans for slipped discs, focusing on a holistic approach to achieve optimal recovery. Each plan is carefully tailored to meet individual needs, combining the latest clinical insights with hands-on care to support long-term healing and resilience. Our physiotherapists evaluate each condition individually and create treatment plans tailored to the patient’s specific needs. Our goal is not only to alleviate symptoms but also to guide and assist our patients in regaining mobility, building strength, and preventing future injuries.
Some key treatment options we offer include:
Manual Therapy
Our hands-on techniques include mobilization and soft tissue manipulation to improve joint mobility, release muscle tension, and alleviate nerve compression. Mobilization helps restore normal joint movement, particularly in the spine, reducing stiffness and improving flexibility in the joint targeted. Soft tissue manipulation targets tight muscles and fascia around the affected area, enhancing blood flow to promote healing and reducing inflammation. These techniques not only provide immediate relief from discomfort but also promote long-term healing by addressing the root causes of the pain and facilitating proper alignment and nerve function.
Spinal Decompression Therapy
Gentle stretching techniques are applied to the spine to relieve pressure on the herniated disc. This promotes disc retraction and improves nutrient exchange, aiding the disc in healing naturally. Significant reductions in nerve pain and improved range of motion are typically experienced after consistent decompression sessions.
Electrotherapy (TENS, Interferential Therapy)
Electrical stimulation is applied to the affected areas to block pain signals and reduce muscle spasms and stiffness in the affected muscles, contributing to pain relief and improved mobility.
Ultrasound Therapy
The use of sound waves on the affected area helps reduce inflammation, increase blood flow, and promote tissue repair, accelerating the healing process.
Radial Shockwave Therapy (RSWT)
Radial shockwave therapy is particularly effective for chronic disc-related pain, promoting tissue regeneration and enhancing healing by sending high-energy sound waves to the affected area.
Postural Correction and Ergonomic Training
Poor posture is a common contributor to slipped disc issues. Postural assessments followed by exercises to improve alignment and correct imbalances help patients achieve and maintain a healthier spinal condition.
Education and Self-Management
In addition to hands-on treatment, we promote patient awareness about their condition by providing personalized education. This includes self-management techniques, strategies to prevent re-injury, and lifestyle modifications. Self-management techniques may include specific exercises to perform at home, ergonomic advice to improve workplace or home environments, and posture correction tips to avoid straining the spine. By empowering patients with knowledge, we help them take an active role in their recovery and reduce the risk of future re-injury.
Exercise Therapy
Last but not least, it is vital to incorporate exercises focusing on core strengthening, flexibility, and postural correction to help stabilize the spine and reduce the risk of re-injury. Additionally, exercises that mimic daily movements are often necessary for patients, contributing to their ability to perform everyday tasks safely, preventing future injuries.
Conclusion
At Synapse Physiotherapy, our goal is to provide a comprehensive solution for patients suffering from slipped discs. Through an evidence-based approach and personalized treatment plans, we aim to achieve long-term relief, restore mobility, and prevent future injuries among our clients. Whether patients experience acute or chronic symptoms, our team is ready to guide them on their journey toward recovery. Contact us today to schedule your consultation and take the first step toward a pain-free life.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.